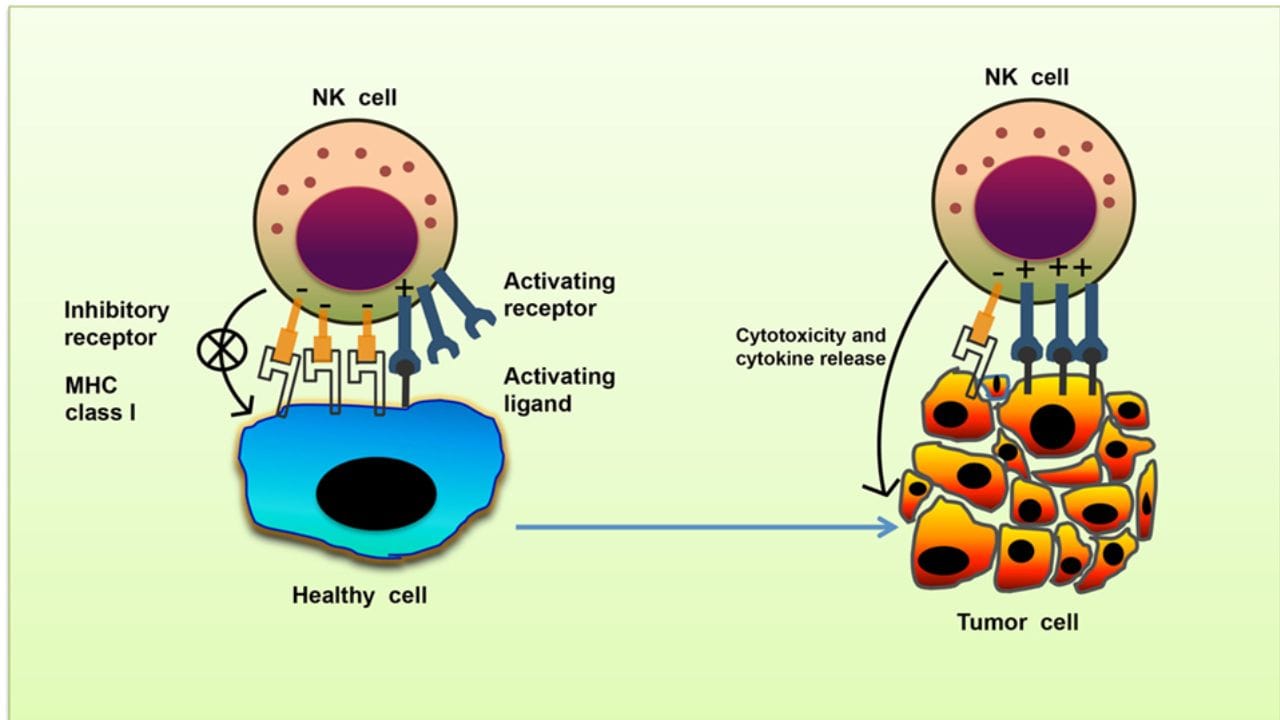
Natural Killer (NK) cells are a crucial component of the innate immune system, acting as the body’s first line of defense against virally infected cells and tumor formation. Unlike T cells or B cells, NK cells do not require prior sensitization to identify and destroy abnormal cells. This makes them an ideal candidate for modern immunotherapeutic approaches, particularly in oncology and chronic viral infections.
One of the most promising applications of this approach is natural killer cell therapy. This treatment utilizes the natural cytotoxic activity of NK cells to selectively target and destroy cancerous or infected cells. These therapies may involve expanding a patient’s own NK cells (autologous) or using donor-derived cells (allogeneic), which are modified and activated outside the body before being reintroduced to the patient’s system.
Clinical studies have demonstrated that nk cells treatment may improve outcomes in patients with certain types of blood cancers, such as leukemia and lymphoma. NK cells can also be engineered to express chimeric antigen receptors (CAR-NK), similar to CAR-T therapy, allowing for more precise targeting of tumor antigens. Unlike CAR-T therapies, CAR-NK cells have a lower risk of causing severe side effects like cytokine release syndrome, making them a potentially safer alternative.
In addition to their anticancer potential, NK cells are also being studied for their role in controlling viral infections, including cytomegalovirus (CMV), hepatitis B, and HIV. Their ability to recognize and eliminate infected cells without prior antigen exposure provides a broad and adaptable immune response. Research is ongoing to better understand how to optimize nk cells treatment protocols and increase their durability and effectiveness in various disease contexts.
NK Cells Therapy: A New Frontier in Precision Immunotherapy
NK cells therapy is emerging as a next-generation immunotherapy that combines safety, specificity, and scalability. Because NK cells do not attack healthy tissues, they present a lower risk of graft-versus-host disease (GVHD), especially in allogeneic applications. This makes them suitable for a wide range of patients, including those undergoing stem cell transplantation or recovering from aggressive cancer treatments.
At the cellular level, NK cells work by releasing cytotoxic granules and signaling molecules like interferon-gamma, which initiate apoptosis in target cells and recruit other immune responses. Advances in cell culture techniques have made it possible to generate large quantities of highly active NK cells in laboratory settings. These developments enable consistent, clinically relevant doses of nk cells therapy, which can now be manufactured under Good Manufacturing Practice (GMP) standards for safe administration.
In solid tumors, natural killer cell therapy presents unique challenges due to the immunosuppressive microenvironment that often surrounds malignant tissues. However, researchers are addressing this by combining NK cells with checkpoint inhibitors, monoclonal antibodies, or cytokine support to enhance their persistence and activity within tumors.
Looking forward, the integration of nk cells therapy with other advanced technologies—such as CRISPR gene editing, mRNA delivery platforms, and artificial intelligence-guided treatment design—may further enhance its precision and effectiveness. Personalized NK cell protocols based on patient-specific tumor markers and immune profiles are already under development.
Institutions like AMSA Biotech are at the forefront of this evolving field, offering high-quality NK cell-based solutions supported by scientific evidence, regulatory compliance, and a patient-first approach. Their commitment to innovation and safety ensures that new therapies are developed responsibly and with the highest standards of care.
In summary, natural killer cell therapy is reshaping the landscape of immune-based medicine. As research and clinical trials continue to validate its effectiveness, NK cell–based treatments are poised to become a standard option for combating cancer and infectious diseases—offering patients new hope and improved outcomes.